AVYXASSIST offers the following program services
Access & Reimbursement Services
Benefit verification
AVYXASSIST is here to help confirm a patient’s insurance coverage, out-of-pocket costs, and any prior authorization needs.
Prior authorization Requirements
AVYXASSIST can help you by providing plan requirements and tracking the status of prior authorization requests.
Appeals support
AVYXASSIST will explain appeal requirements and monitor the status of submitted appeals for your patients.
Claims support
AVYXASSIST can provide billing and coding guidance as well as assistance with claim denials and underpayments.
Access & reimbursement services: Who’s eligible?
- Patients with commercial, Medicare, Medicaid, or other government insurance plans
- Patients prescribed an AVYXA product
- Please contact a Patient Access Specialist to learn more about any of our AVYXASSIST services
There are no financial requirements.
Access & Reimbursement Services
Benefit verification
AVYXASSIST is here to help confirm a patient’s insurance coverage, out-of-pocket costs, and any prior authorization needs.
Prior authorization assistance
AVYXASSIST can help you by providing plan requirements and tracking the status of prior authorization requests.
Appeals support
AVYXASSIST will explain appeal requirements and monitor the status of submitted appeals for your patients.
Claims support
AVYXASSIST can provide billing and coding guidance as well as assistance with claim denials and underpayments.
Access & reimbursement services: Who’s eligible?
- Patients with commercial, Medicare, Medicaid, or other government insurance plans
- Patients prescribed an AVYXA product
There are no financial requirements.
REFERRALS TO 501(c)(3) FOUNDATIONS
When appropriate, AVYXASSIST can connect patients to charitable foundations when they are not eligible for other services. Contact an AVYXASSIST Patient Access Specialist today to learn more.
Who’s eligible?
Patients prescribed an AVYXA product 501(c)(3) foundations may have their own financial requirements.
Free product assistance
AVYXASSIST may offer free product assistance to eligible uninsured or underinsured patients who do not qualify for other assistance. Contact an AVYXASSIST Patient Access Specialist today to determine eligibility. Terms and conditions may apply.
Who’s eligible?
- Patients prescribed an AVYXA product
- Patients who meet financial criteria
All patients who meet the eligibility requirements.
Bridge supply
For existing patients administered an AVYXA product that has a change in benefits, or an issue with coordination of benefits and their insurance is not covering.
Who’s eligible?
- Patients with commercial, Medicare, Medicaid, or other government insurance plans
- Patients prescribed an AVYXA product
- Scheduled appointment in 5 days or less
There are no financial requirements.
Product replacement
This program allows physician offices or hospital outpatient departments to receive replacement product when specific situations occur, and eligibility criteria are met. Contact a patient access specialist for eligibility criteria.
Contact us:
For assistance, please call an AVYXASSIST Patient Access Specialist at 866-939-8927, or email reimbursement@avyxa.com.
Copay assistance
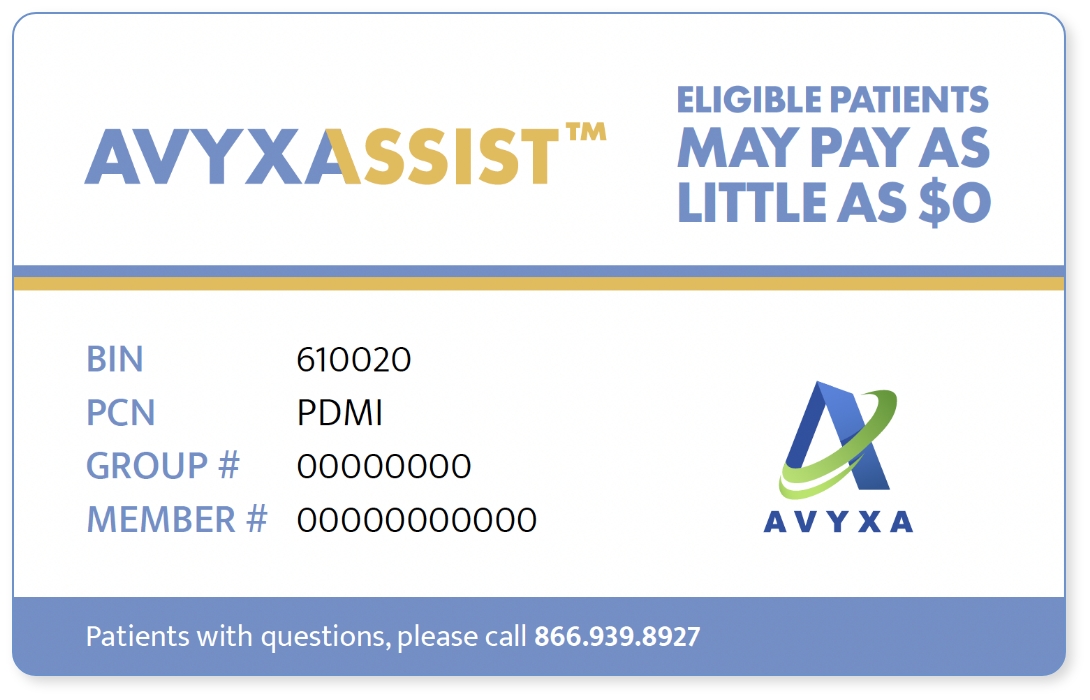
Commercially eligible patients prescribed an AVYXA product may pay as little as
$0
per dose*
There are no financial requirements.
* up to $25,000 per patient, per drug.
We work closely with HCPs and patients to remove financial barriers for eligible patients in need.
AVYXA understands that your personal and health information is private and will only use your information in accordance with our Privacy Policy. The information you provide will only be used by AVYXA and parties acting on its behalf to send you requested product and/or related product information, copay program information, offers, and services.
